Transform Health Insurance with Data-Driven Insights
Coverage Cost-Effectiveness and Outcome Insights for Health Insurance
How does your health plan decide what products, drugs, and services to cover?
$4.3T
U.S. Healthcare Spending
9.1%
Annual Growth Rate
$1.5T
Drug & Device Spending
The Innovation Gap
Despite being one of the most important areas for U.S. Healthcare innovation, nobody is really doing anything about it
See Our SolutionHealth plans issue medical policy to set criteria for coverage of services, drugs, and medical devices
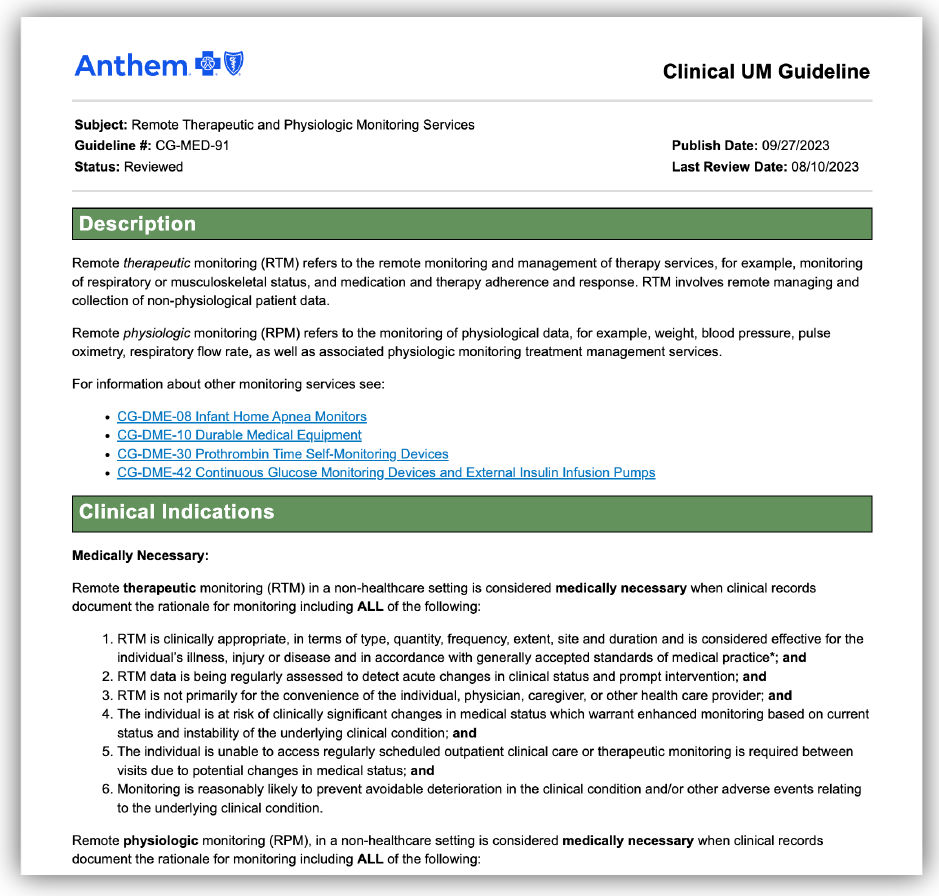
Medical policy or utilization management (UM) policy is the criteria by which health plans officially cover a service or product
-
Eligible Diagnoses
Specific conditions that qualify for coverage
-
Specific Testing Requirements
Necessary diagnostic evaluations
-
Required Service Elements
-
Documentation Requirements
-
Treatment Pathway Requirements
Health plans use medical policy guidance to promote specific business goals
Stated Goals
Evidence-Based Practice
States the plan's view of appropriate clinical practice and supports evidence-based practice
Authorization Guidance
Provides guidance to clinics on prior authorization requirements
Cost Control
Prevents wasteful utilization and spending
Unstated Goals
Administrative Friction
Creates administrative burden for clinics and patients to reduce cost via friction
Legal Protection
Provides legal cover for denying services
Cost Barriers
Creates barriers to higher cost services
Cost Routing
Routes patients to lower cost services and products, first
Health Plans Issue Medical Policy Guidelines Via
Haphazard, Expensive, and Manual Processes

Boom! Health Analytics provides a research product For Payors

Boom! Health Analytics
What?
Online, Subscription Research Product
For Who?
Health care risk bearing entities and health plans
How?
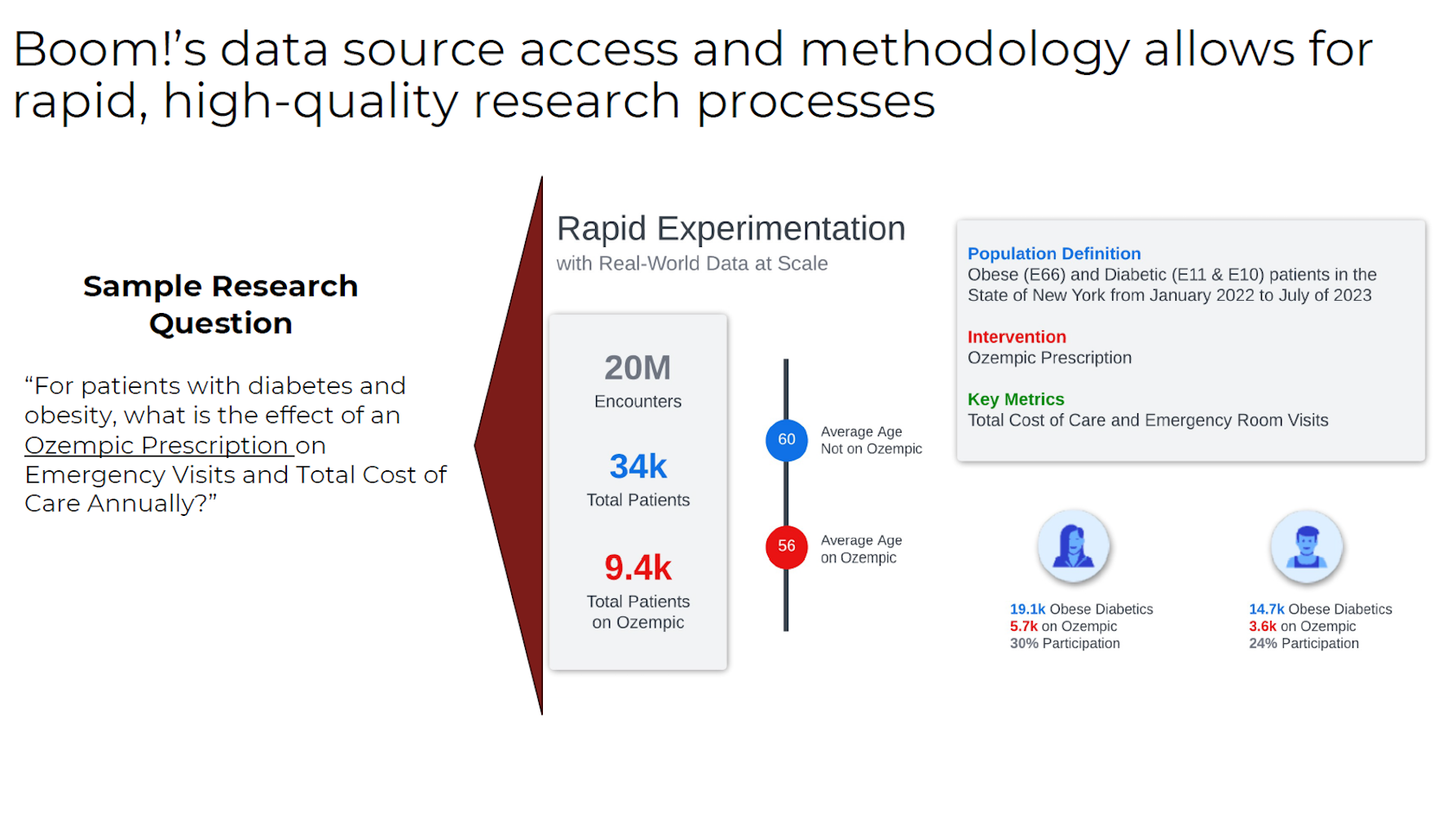
Contractual Access to Massive, National Claims Data & Machine Learning Driven Insights, Validated by Qualified Humans
Why?
To influence Medical Policy and Coverage to help health plans gain insight to reduce cost, predict cost, and improve health
To accelerate the adoption of impactful technologies that can advance human health
We Provide Payors With a Research Product For Cost-Effectiveness & Coverage Analysis for Health Plans
Key Questions We Answer
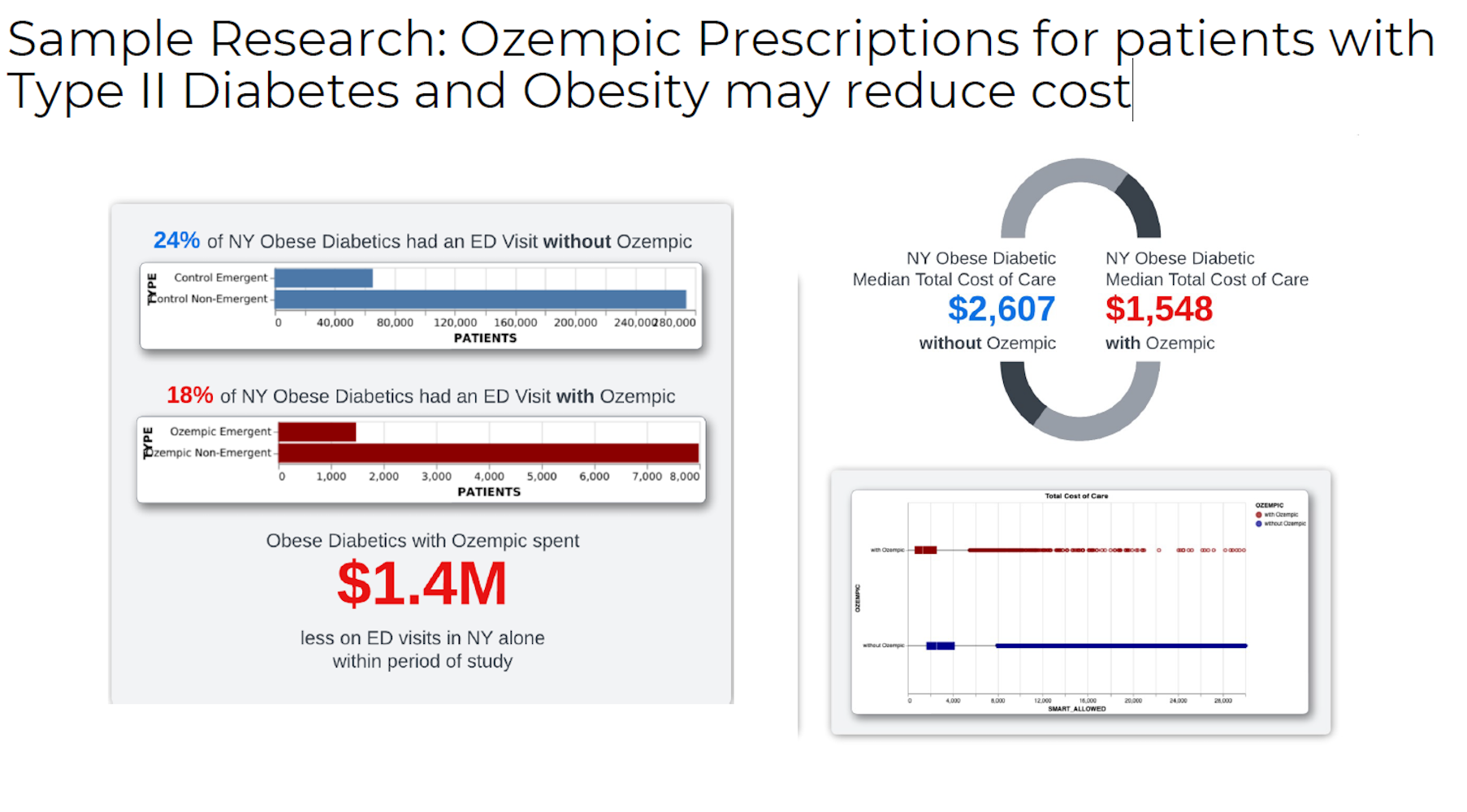
Coverage Criteria
What new emerging technologies, drugs, care models, and services should I cover and by what criteria?
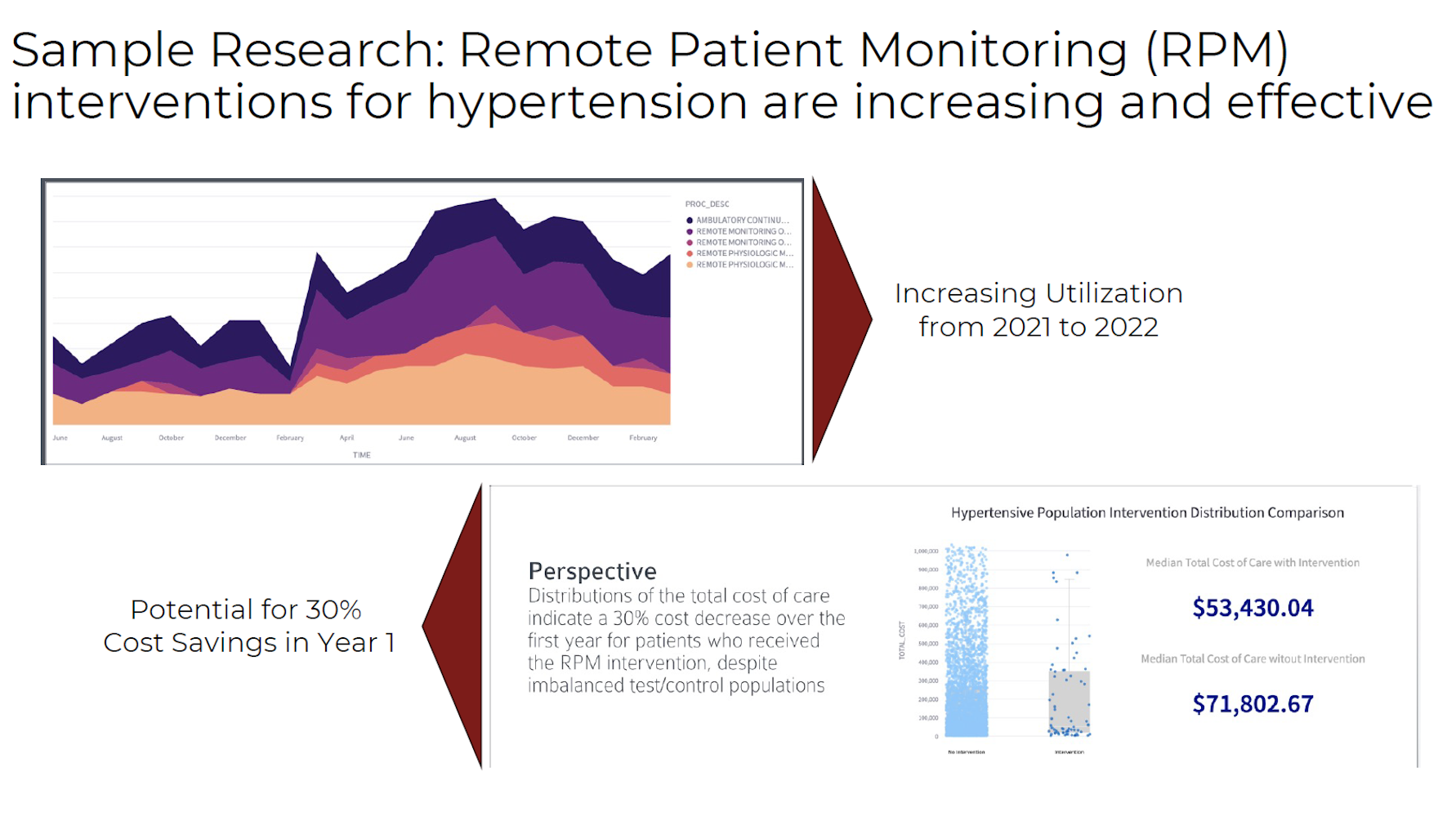
Network Incentives
What technologies and services should I promote and incentivize in my provider network and vendors?
Impact Assessment
How can I assess the potential impact of coverage decisions faster?
ROI Analysis
At what payment rate can I expect a return on investment for a particular benefit?
Timeline Projection
In what timeframe can I expect a return from a particular technology, drug, care model, or service?
Cost Trends
What areas of cost are changing most rapidly year-over-year?
Our multi-payor type claims data lake allows for valid and robust analysis
Patient Journey Structured Claims Data Source
Patient Encounters
Patient Journeys
Years of History
Real-time Updates
Our research methodology is academic-grade and
designed to produce valid and generalizable insights
Claims
Database
Engine
Identification
Statistical
Investigation
Feasibility
Logic Test
Product
Reports
Our insights provide key benefits to payors
Predictability of Cost
Identification of Rising Cost Areas
Analyzing trends and patterns to identify key cost drivers
Opportunities for ROI
Areas of Interest for HEDIS/STAR
Strategic focus areas for quality improvement
Data-Driven Insights
Discover how our research methodology delivers actionable healthcare insights
Ready to Transform Healthcare?
Join leading healthcare organizations using our platform to drive better outcomes.
Start Free Trial